ABOUT PRIMARY HYPEROXALURIA TYPE 1 (PH1):
It’s okay to have questions.
You may be overwhelmed to receive a diagnosis of primary hyperoxaluria type 1 (PH1) and want to know more about what it means to have this disease. You aren't alone. This is a resource for answers to common questions about PH1.
What is PH1?
Primary hyperoxaluria is a rare, inherited disease that causes the overproduction of oxalate. In a healthy liver, oxalate is present only in small amounts. As oxalate is not used by the body, it is removed by the kidneys.
PH1 Patient Perspectives: Describing PH1

PH1 causes the liver to make too much oxalate.
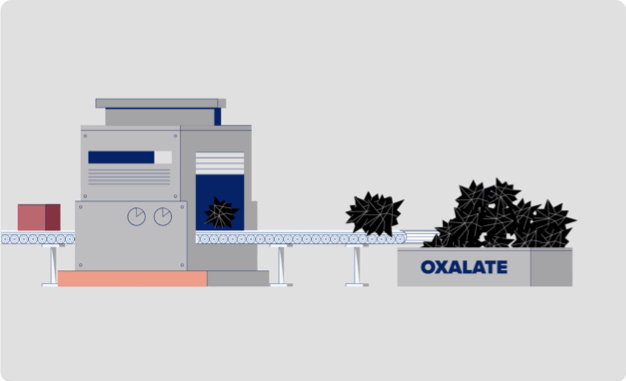
In PH1, oxalate is overproduced due to a broken process that involves the liver enzymes called glycolate oxidase (GO) and alanine: glyoxylate aminotransferase (AGT). Think of your liver as a factory, and these enzymes that work there as machines that help your body make or break down substances. Watch how this happens, below:

Because PH1 is caused by oxalate overproduction, your doctor will monitor the levels of oxalate within your body.

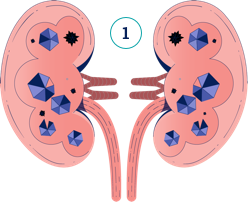
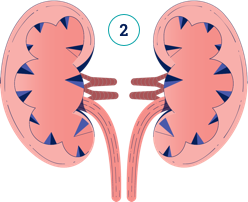
What can happen when oxalate is overproduced?
In PH1, oxalate is constantly being overproduced by the liver, and the kidneys cannot keep up with removing it. Watch the video below to understand how damage can occur.

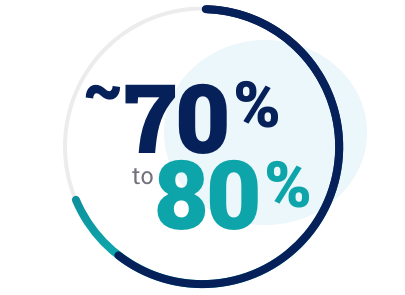
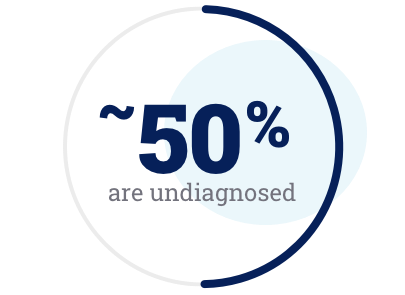
In PH1, oxalate is constantly overproduced and can cause the disease to progress, meaning that it gets worse over time. Diagnosing PH1 as early as possible can help you take steps to manage it.

What are the signs to look for in PH1?
Although kidney stones are the most common and often the first symptom of PH1, not all people with PH1 will have stones. When you have PH1, your kidneys are at risk for damage even if you do not have stones.
PH1 may present in a number of ways:
Having kidney stones,
even only one, as a child
Having repeated kidney stones (recurrent kidney stones)
Finding crystals in kidney tissue during a kidney test (nephrocalcinosis)
Kidney failure (end-stage renal disease or ESRD)
Not growing sufficiently as a baby (failure to thrive)
There was just blood in his urine.
He had
no other symptoms, but you could see that he was in pain. I remember he had a lot of stones in his kidney when he first got diagnosed.
What are some of the symptoms I could experience?
Kidney stone symptoms can include:
- Pain in the back or sides of the body
- Pain when you urinate
- Blood in the urine (hematuria)
- Urinary tract infections (UTIs)
- Passing stones in urine
If you think you are experiencing these symptoms, consider contacting your doctor.
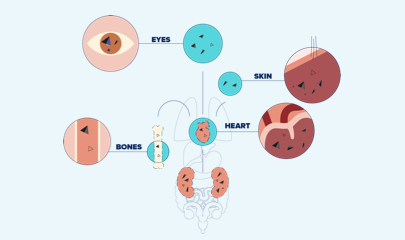
Symptoms of end-stage renal disease (ESRD) can include:
- Producing little or no urine
- Feeling ill and tired
- Loss of appetite, nausea and vomiting
- Pale skin color
- Swelling of the hands and feet
- In PH1, poor kidney function that can lead to oxalate spreading throughout the body
If you think you are experiencing these symptoms, consider contacting your doctort. By keeping track of your kidney health, you and your doctor can make more informed decisions about your care.
Can someone in my family have PH1 too?
PH1 is an inherited condition, meaning that it is passed down within families. It is important that family members, especially siblings, of a person with PH1 consider getting tested for the disease via a genetic test.
PH1 Handbook
You can customise and download your own PH1 Handbook, which provides an overview of PH1 management, monitoring, and more.
next

PH1-CAN-00002 | April 2022